Oral-History:Leslie Geddes
About Leslie Geddes
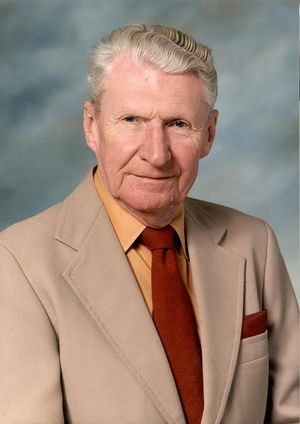
Geddes was born in 1921 in Scotland, and moved with his family to Canada in 1926. He had an early and continuing interest in combining electronics with medicine, which led him to bioengineering. He was at McGill during World War II as a soldier/student, gaining a degree in Electrical Engineering and learning about physiology. He helped H. H. Jasper make the first electromyography in this period. He worked at the Montreal Neurological Institute and McGill after the war, till 1952, as a split-discipline instructor, gaining his Masters of Engineering from McGill in 1953 with a thesis on A Line Operated Electromyograph. He moved to Baylor in 1952 and stayed there till 1974; got his PhD in physiology there in 1959; moved to Purdue University in 1974 and stayed there. In the 1950s he was developing the Physiograph (with his mentor Hebbel Hoff), developing diagnostic equipment for polio, founding a summer program to teach modern physiology and experimental electronics; in the 1960s and later working on electric defibrillators; consulting with NASA on physiological monitoring of astronauts; working to diminish electrical hazards at hospitals; figuring out how to measure blood pressure by oscillometry; many papers on the history of science. At Purdue, he helped develop the Biomedical Engineering Center, later turned into the Biomedical Engineering Department. He was involved in the IEEE Engineering in Medicine and Biology Society and the professional group on Medical Electronics.
About the Interview
LESLIE A. GEDDES: An Interview Conducted by Frederik Nebeker, IEEE History Center, 13 October 2000
Interview #406 for the IEEE History Center, The Institute of Electrical and Electronics Engineering, Inc.
Copyright Statement
This manuscript is being made available for research purposes only. All literary rights in the manuscript, including the right to publish, are reserved to the IEEE History Center. No part of the manuscript may be quoted for publication without the written permission of the Director of IEEE History Center.
Request for permission to quote for publication should be addressed to the IEEE History Center Oral History Program, IEEE History Center, 445 Hoes Lane, Piscataway, NJ 08854 USA or ieee-history@ieee.org. It should include identification of the specific passages to be quoted, anticipated use of the passages, and identification of the user.
It is recommended that this oral history be cited as follows:
Leslie A. Geddes, an oral history conducted in 2000 by Frederik Nebeker, IEEE History Center, Piscataway, NJ, USA.
Interview
Interview: Leslie A. Geddes
Interviewer: Frederik Nebeker
Date: 13 October 2000
Place: Purdue University, West Lafayette, Indiana
Childhood, family, and educational background
Nebeker:
You were born the 24th of May, 1921, in Port Gordon, Scotland.
Geddes:
Correct.
Nebeker:
Scotland has as rich an engineering tradition as any country, I think.
Geddes:
Yes. Glasgow was the prominent place.
Nebeker:
Was there any engineering in your family background?
Geddes:
No.
Nebeker:
Tell me a little about your family.
Geddes:
They were mostly from Aberdeen, which is up in the highlands. My father was a wood merchant. He left Scotland and immigrated to western Canada before World War I.
Nebeker:
How old were you at that time?
Geddes:
This occurred before I was born. He returned to Scotland married my mother. I was six when I came to Canada. It was about 1926 and I had my schooling in Canada.
Nebeker:
You were just about to begin schooling in Scotland?
Geddes:
My father was in World War I. He left Canada in 1914 and was in the Royal Flying Corps, which was the predecessor to the RAF. The Duke of Windsor was the Adjutant at that time. Then in 1918, he left the service and married my mother. I was born in 1921. He returned to Canada without us and established a position at the Northern Electric Company. We followed in 1926 or so and landed in Montreal.
Nebeker:
What was he doing for the Northern Electric Company?
Geddes:
The Northern Electric, is the analog of Western Electric. It is the Canadian equivalent. which made telephones. He was in telephone and cable business and he worked on the early traffic signals. Northern Electric started to branch out from making telephones into other areas making Hammond Organs and radios. During the early days of radio in the late ‘20s they were making vacuum tube radios. That is how he could bring home a vacuum tube, or a capacitor, or a resistor for me.
Nebeker:
Where were you living then?
Geddes:
Just outside Montreal in a little place called St. Lambert, which is across the river from Montreal. We lived there until I went to McGill in 1940. In 1939, when I graduated from high school, the War started. I went to work at the Northern Electric Company for a year. From the moment I began working for Northern Electric, I was in the Inspection and Testing Laboratory for testing telephones, breaking them and testing their electrical characteristics. A man of about sixty years old ended up working for me. I looked at him and said, “I don’t want to be that man when I’m that age. I have to go to college.” So I went to college.
Nebeker:
Earlier you mentioned you had an interest in amateur radio.
Geddes:
Yes. I was making crystal sets in the 1926, ‘27, and ‘28 era. In Montreal, we could receive WLW in Cincinnati. It had an output of 500,000 watts at that time, so they put out a pretty good signal. Then in the ‘30s, I started to build radio transmitters and fiddled around before I had a license. I built my own ham station and got licensed in 1935; my call letters were VE2LR.
Nebeker:
Was your father involved in this also?
Geddes:
No. It was just my own hobby, but he was a supporter. He brought home all kinds of hardware and I would put it together and build radios, transmitters, and so on.
Nebeker:
Were you able to pick up any stations from some distance?
Geddes:
Yes. I went on the air in 1935 and I had to go off in ‘39 because the War came to the British colonies in 1939. From 1935 to 1939 my call letters were VE2LR. I ended up with a 500-watt transmitter, which is a pretty good-sized radio station using telephony as well as Morse code. I talked to hams all over the United States. I speak Spanish, so I had calls from Cuba, South America, and Mexico. From the European countries, I had calls from Germany, France, and Spain.
I would get up at four o’clock in the morning when the reception was good and transmit until I went to school at nine o’clock. School was across the street, so it was very convenient.
Nebeker:
It sounds like it was quite an activity for you.
Military service and undergraduate studies in electrical engineering, communications
Geddes:
Yes. I went off the air in 1939 and went to college the next year enrolled in electrical engineering. Then I entered military service, even though I was in college. I had to serve in the Army, and I was a private while I was at school. I decided that was for the birds.
I did the wrong thing as far as being a military person is concerned. I volunteered for some activity with a great man who was a one-legged major who had had his leg blown off in World War I. He was an instructional officer in bridge building and demolitions. I became a demolitions expert under him. I was blowing up bridges. I spent part of the summers in military camp. I was in uniform all during the time I was in college.
Nebeker:
You were allowed to continue your education, but you had to be in the service?
Geddes:
Yes. I soon became a second lieutenant and then I was a lieutenant. Every summer I had to go to military camp. At other times I was a training officer in what you would call the O.T.C.
Nebeker:
The Canadian equivalent of that.
Geddes:
Yes. COTC was what it was called: Canadian Officer’s Training Corps. I was on duty all the time except when I had two or three weeks off in the summer. Then I would work for the Canadian Broadcasting Corporation. I was a transmitter engineer for CBM in Montreal. Then I was a studio engineer for two summers during my two or three week leave in the summer.
Nebeker:
So that’s where your audio engineering was further developed.
Geddes:
Yes. It was a very exciting job being a studio engineer. I had to take out the U. S. commercial and put in the local commercial. The Bing Crosby Show was a fantastic experience. I would receive a seven-page telegram, five minutes before airtime for the commercial that they’re going to give. I had one headphone listening to the U. S. and the other was listening to the local announcer. All the while I was looking at the clock, and Crosby were never on time. I learned the value of a second. I enjoyed that, as a matter of fact, and did that until the end of the War.
During the latter months of the War, I was a volunteer at the Montreal Neurological Institute. At the end of the War I was an instructor in Electrical Engineering at McGill.
Nebeker:
Even before you completed your degree?
Geddes:
Yes, this was before I completed my degree—I volunteered. In 1944, I was working with H. H. Jasper making the first electromyograph. Then I worked in EE making hardware for the electronics labs, all the time wearing a uniform. I always had lots of activities going on.
When the hostilities ended in Europe, I resigned my commission. I had that option. I got married and went to work at McGill as an instructor in EE and an instructor in neurophysiology at the Montreal Neurological Institute, which is the Department of Neurology and Neurosurgery at McGill.
Nebeker:
In the EE program, are you interested mainly in communications/radio engineering?
Geddes:
Yes. They didn’t have a Ph.D. at that time in electronics, as it was called. Electronics was considered an unworthy pursuit because they thought you couldn’t get a job in electronics, so we had to take all the power courses. I took all the power courses and all the electronics courses.
Graduate studies, publications, and employment in medical electronics
Geddes:
I had started my graduate studies in my last year and I was taking all these courses at night.
Nebeker:
How did you become interested in physiology?
Geddes:
Well, I was interested in medical electronics.
Nebeker:
There wasn’t much of that in 1945.
Geddes:
No. My first paper described the RC AMC electromyograph.
Nebeker:
I have a list of your publications.
Geddes:
It was published in April 1945. I was working on it in 1944. It was quite an elegant device with a differential amplifier, a loud speaker, and oscilloscope. There were a lot of soldiers returning home with nerve injuries. You could diagnose nerve injury with the electromyograph—just place some electrodes in a muscle and one could detect a characteristic electrical activity. That was what I was doing during the last year of the War at McGill.
I then went to the Montreal Neurological Institute in 1945 as an employee and stayed there until 1952. I worked in the Electrical Engineering Department from 1945 to 1946. I was one of the early biomedical engineers. They didn’t know what that was at the time. It was all medical physics at that time. I was responsible for the operating room equipment and for the electroencephalography laboratory. I gave a course in electronics to the fellows and residents. It was a fun time.
Nebeker:
One might think that with your amateur radio experience that you might want to go into radio engineering. Yet, somehow you had an interest in applying electronics to medicine.
Geddes:
Yes. Some of my relatives had been physicians. Sir Auckland Campbell Geddes was a physician and my father’s uncle was a physician. So there were several physicians in the family; but I became interested in medical electronics. This was what made me say, “I want to apply electronics to medicine,” being possible with my electronics experience and the ham radio experience.
Nebeker:
Who were the people that you worked with in this period?
Geddes:
The head of the Institute was Wilder Penfield, who was the world-renowned specialist in epileptic surgery. He pioneered the surgical technique. Epilepsy is a dysrhythmia of the brain and it produces a convulsion. One can locate the origin of this convulsion electrically by putting electrodes on the exposed brain. If one takes out that focal area, one cures the epilepsy. So, one needed a six-channel recording with three channels for each side of the head. The electrodes that I made and the equipment were shown in the Scientific American of 1948. The electrodes I made were on the cover. I have pictures of the equipment. It was used until about five years ago.
Nebeker:
Is that right?
Geddes:
- Audio File
- MP3 Audio
(406 - geddes - clip 1.mp3)
Yes. Vacuum tube equipment in the operating room. It lasted quite a while.
I stayed at McGill until 1952 teaching, servicing equipment, building hardware for research, building scopes, stimulators, all those kinds of things.
I had met some people at McGill who went to Texas. From 1950 to ‘52, they goaded me to come to Houston. The polio epidemic was on and they needed an engineer to build diagnostic and therapeutic equipment, controllers, and measuring devices. For two years they courted me. In 1952 I went to Houston with a green card. Interestingly enough, to get admitted into the United States I had to have a chest X-ray to show that I did not have TB. I also had to have a blood Wassermann result to show that I did not have syphilis. The result had to be on the x-ray film.
On Labor Day weekend of 1952, my father drove me down to the border. I had already bought a car in Malone in New York State, and the dealer had delivered it at the border. I went to the border, then through customs and immigration. The immigration officer said to me, “Are you going to the United States to take a job?” I said, “Yes. I have a position there.” He also said, “Do you know you’re displacing an American?” I said, “No, I didn’t know that.” He said, “Do you know what would happen if you didn’t have a job?” I said, “No. I don’t.” He said, “You would become a ward of the state, and I can deny you entry in the United States for either reason.” I said, “Why is that?” He said, “If we don’t like somebody for some reason, we can use one of these two reasons or both of them.” So I thought, “I’m finished. I’m through.” Anyway, he said, “Good luck.” Then I got into my new car and the immigration siren blasted. I looked up and thought, “What the heck did I do?” The officer came over and said, “Come back here.” I said, “What did I do, sir?” He said, “Do you know what weekend this is?” I said, “Yes.” He said, “Do you know how many people are going to be killed on the highways?” I said, “I don’t know.” He said, “Five hundred. Please drive carefully.” I don’t know whether he was testing me or not, but that was my introduction to the United States.
Nebeker:
I see on your CV that you received the Master of Engineering from McGill in 1953. Is that right?
Geddes:
Yes. I had taken all of my courses, and I was so busy at Baylor Medical School I did not have time to write my thesis. When I was a Baylor, I was a biophysicist. They called me a biophysicist and I was making laboratory equipment. I had taken all my courses at McGill, and I had done all my research, but I hadn’t written my thesis and it took me a little while to get my thesis written.
Nebeker:
What was the subject of your Master’s thesis?
Geddes:
A Line Operated Electromyograph. All the electromyographs were high gain devices that were working down at the noise level, and they had to operate from batteries at that time. I figured out how to make very clean power supplies to eliminate the batteries. All electroencephalographs, electrocardiographs, electromyographs were all battery operated during that time. I wrote my thesis and presented it, and got my Master’s Degree from McGill.
Employment, research, and Ph.D. studies at Baylor
Nebeker:
Tell me about your work at Baylor in the first years.
Geddes:
It was interesting. I was hired to make diagnostic equipment for a place called the Southwest Polio Research Center, SWPRC. It was a place that was full of polio patients in iron lungs. One of the problems of keeping these people alive was how to set the iron lungs to provide proper blood oxygenation. We had to make pulmonary function testing equipment and oxygen saturation devices, oximeters, CO2 analyzers, and the like.
Nebeker:
This equipment couldn’t be bought off-the-shelf in those days?
Geddes:
No. The research sponsor was the National Foundation for Infantile Paralysis, NFIP. At that time, they funded the Southwest Poliomyelitis Research Center. I was a biophysicist with a joint appointment at the Physiology Department at Baylor Medical College; SWPRC was a division of Baylor. It was part of their Pediatrics Department because it was children who got polio.
I entered the Ph.D. program in 1954 or 1955 in physiology with a minor in pharmacology.
Nebeker:
I was curious about that. You had enough of a background in physiology or biology generally that you could enter the Ph.D. program?
Geddes:
Yes. McGill is very good at giving a good rounded education. I started my PhD program around 1954 or 1955. What I was doing at Baylor was to build the Physiograph. The teaching of physiology was in the dark ages then. Everybody used a smoked drum, the Ludwig kymograph, to record only mechanical events. So, I built the Physiograph on a modular electronic system that permitted recording many different types of physiological events. This is where my Northern Electric experience and ham-radio experience paid off. The Bell telephone system has a philosophy that any new device that is made must fit with the old system—it must be compatible. So a modular concept was the keynote for the Physiograph which had a transducer, an amplifier, and a display device. One could connect a variety of different compatible transducers to the amplifier, which energized the transducer and amplified its signal. One could then have the event written out on a graphic recorder, or displayed on an oscilloscope, or heard by a loud speaker. We displaced the smoke drum kymograph around 1955 or so.
Nebeker:
Was this an ink graphic recorder that you created?
Geddes:
Yes, exactly, with attachments. For the oscilloscope, one could take the power amplifier out of the Physiograph and plug it into the oscilloscope. It would drive the transducer and you’d have a high-speed display. I can show you some pictures of that, if you want.
Nebeker:
Would you take photographs of the oscilloscope if you needed a permanent record?
Geddes:
Yes, with a Polaroid camera. Or sometimes we would put the sweep on repetitive and place a transparent celluloid film on the CRT and trace the event on the film.
National Heart Institute training program, 1956-1974
Geddes:
This system created so much attention that the NIH funded us for a training program which originated in the following way.
My mentor (Hoff) and I were sitting in the Washington National airport about 1955 or so. My mentor was a great person—a Rhodes scholar, M.D. from Harvard, Ph.D. from Oxford; he had all the credentials. He said, “You know, the U.S. is not turning out enough scientists.” We had three hours to kill, and we obtained a magnum of champagne and began feeling great. In response to his statement I said, “Yes. And if we don’t train scientists, the Russians will do it.” That was the magic term then. We sketched our ideas on the restaurant menu.
On arriving home, we applied to NIH to teach modern physiology. The program was entitled, Classical Physiology With Modern Instrumentation. The concept was like “Shakespeare in Modern Dress”. We received the funds for a six-week summer course with stipends for tuition and expenses. We had people from all over the world as well as the United States. This National Heart Institute training program was the longest single managed training grant that NIH had ever funded up to that time. It ran from 1956 to 1974—eighteen years. We trained about one thousand people. It was a back-breaker in the hot Houston summertime, but it was fun. We had all kinds of interesting people. We had the Surgeon General from the Japanese Navy; we had the commander of the Japanese Air Force, the Japanese Air Self-defense Command in the class. It was an amazing collection of people—people with the highest civilian rank equivalent to general.
Nebeker:
You and Hoff taught the course?
Geddes:
Yes, with a few student assistants.
Nebeker:
All these summers?
Geddes:
Every summer. Electronics in the morning, physiology in the afternoon. An hour, hour and a half electronics lecture, and then a lab in electronics. The same schedule in the afternoon. It was a great, great experience.
Hebbel Hoff as mentor
Nebeker:
I would like to hear something about Hoff. How you first met him?
Geddes:
He was professor of biology at McGill when I was there. I didn’t know him at that time, but he knew about me. He knew I was headed for military service. He knew before I did and he was following my career. He must have left McGill around 1947 or 1948. I was at McGill and graduated before that time. He wanted me to come and work for him in the biology department before he left for Houston. He was a physiologist who was taught by the giants: Sherington and Adrian and all those people.
Nebeker:
Was he a very quantitative researcher?
Geddes:
Yes. A very exacting person. He could analyze any problem by taking it down to its simplest elements.
Nebeker:
It was a case of he knew about you but you didn’t know him at McGill.
Geddes:
He was on the Military Advisory Committee and he was the one who wanted to get me into the Canadian Army. I had other plans, but he had never given up on me. He was an elegant teacher—he was an orator supreme. He could make the difficult seem very, very simple and reasonable. He always lectured with a cup of coffee. He would walk up and down drinking his coffee in his hand. He would put it down, write something on the black board, and then pick up his coffee. Just a tremendous orator. Very charismatic—a role model. All the time I was at Baylor, I went to every one of his physiology lectures. In the beginning, when I was taking my Ph.D., I would go to his lecture, although I had taken the course. He would say about ten minutes into the lecture, “Now Mr. Geddes is going to take over,” and he left.
Nebeker:
Had he warned you about this?
Geddes:
No. He just did it. We were making a movie on open chest ventricular defibrillation in the Dental School in Houston. We got into it about five minutes and he said, “This is your Ph.D. examination rehearsal. Take over.” He knew I could do it. I didn’t know I could do it. He just threw me into the water and I had to swim. I learned very quickly what you have to do to survive. When you are learning something you have to learn it so that you can tell it to somebody else; if you can do this then you know the subject. So, he taught me how to teach.
Ph.D. research in experimental physiology; equipment and experiment design
Nebeker:
Tell me about your Ph.D. program and your research.
Geddes:
My research was to not only build the equipment but to design the physiology and pharmacology lab experiments for medical students. We were designing and building the equipment and doing the experiments the day before, and wrote it up to give it to the medical students the following day. We covered the vascular system, the renal system, the nervous system, the gastrointestinal system and the respiratory system—all the systems. I still have a copy of the laboratory manual. This is the Spanish edition and here is an English edition.
Nebeker:
This is experimental physiology.
Geddes:
That was half of my thesis. Half of my work was to build the hardware, and the other half was to design the experiments and make them work. Notice that the pages are printed to the size of a Physiograph record page. It’s fanfold paper and you will see records in there. I had to learn a lot fast.
Nebeker:
A whole range of types of measurements.
Geddes:
Yes. I had to design and build all the transducers, make them work, and write the experiment for them.
Nebeker:
So from the beginning of your career, you have dealt with a whole range of instrumentation. Was it in 1959 that you completed your Ph.D.?
Geddes:
Yes. The other part of the summer course, by the way, was experimental electronics. This was the morning session for the course and the afternoon was the physiology course. All very basic stuff: vacuum tubes, transistors, and RLC circuits—all those kind of good things. I also wrote an electronics lab manual.
In 1944 while volunteering at MNI in Montreal, I married Penfield’s nurse. She was a great nurse. She was a Winnipeg lady who was a scrub nurse in the surgery. I married her in 1945 and we fell apart in 1952 when I went to Texas. She came down to Texas in 1953, stayed a year, then we were divorced. I was single from 1954 to 1962 when I married my present wife, LaNelle. After the divorce I had lots of time. I didn’t have any obligations. So that’s how I could spend all the time on my work.
Nebeker:
Your son was born later?
Geddes:
My son was born to my first wife in 1947, and in 1954 she took him back to Canada. I have seen him only once since then.
Hebbel Hoff and lab research; graphic recorder without vacuum tubes
Nebeker:
It sounds like you were very busy with all the course work and Ph.D. program. How was Hoff in the laboratory?
Geddes:
Excellent. Absolutely a superb surgeon. He had wonderful hands.
Nebeker:
How about electronics? Did he know that?
Geddes:
He knew what could be done easily and what was difficult. He had a great appreciation for what I did. I helped him in his research. He was a pioneer in the nervous system’s control of respiration. I built the hardware and worked with him very, very closely. He published the classical papers on how the medulla integrates all the information to control breathing. That was when I first went down to Houston. We built the first graphic recorder that had no vacuum tubes. It was a transformer (a magnetic amplifier).
Nebeker:
The signal strength was strong enough to move the pens?
Geddes:
Yes. In the magnetic amplifier there were two coils and they were bucking; another coil changed the flux linkage. It was called a magnetic amplifier. We built the transducers with enough output to change the flux and the output of the device would operate a pen directly. But it had a slow response time. It was a sixty-cycle carrier system. The response time is not good enough to reproduce respiration accurately. That got us onto using vacuum tubes and then got us onto the Physiograph.
The Physiograph and defibrillation in medical practice
Nebeker:
I am curious about the state of the art at that time. One couldn’t buy an amplifier off the shelf that would do the job?
Geddes:
There were no rapidly responding recorders. The only graphic recorders were in the electrocardiograph and they couldn’t respond rapidly enough. We had to build amplifiers that were differential, first of all. They had to be immune to sixty-cycle interference with a high common mode rejection ratio. The amplifier had to have enough output to drive a pen, which needed about twenty watts. I designed the whole system and made it modular so one could change the transducer and obtain a graphic record of electrical activity, mechanical activity, blood pressure, respiration, heart sounds etc. It was a modular system.
Nebeker:
So, people who took that summer course, for example, and then wanted to go back and do that sort of thing in their own labs, could they buy the equipment?
Geddes:
You put your finger on it. At the beginning, no. However, there were three technicians who worked for me building the Physiograph. Huntly Millar was one of them and he formed the E and M Instrument Co. There was also a mechanical technician and an electronics technician. They went out and formed the company called E&M Instrument Company (Electrical and Mechanical). They started to build the Physiograph and sell them to new graduates at first. They didn’t do very well and E&M was bought by Narco Biosystems. That put some capital, management and marketing into the company. But it wasn’t doing real well until they figured out that the salesmen sold Physiographs to people who didn’t know enough physiology. So we developed a training program for all the salesmen. They went out and sold the Physiographs and gave the buyers a lab manual and taught them how to do the physiology. This created a market. I didn’t get anything for the Physiograph. It’s not even patented. Narco Biosystems was bought a few years ago by a company in Austin, TX.
Nebeker:
There must have been other instrument companies in this post-War period.
Geddes:
Albert Grass started to make a polygraph recorder along about 1958 or 1959. First of all, the Physiograph wasn’t met with any success at all by the physiologists. They said, “This is terrible. It makes learning too easy. You learn best by failures, and by defeat, and by working very hard. The Physiograph guarantees success.”
Just after we started using the Physiograph we made a time analysis, and with the old smoked drum, it took two hours of a three-hour period to get set up to get to the physiology experiment. As a matter of fact, people used to sharpen their fingernails, and to get the records, they would draw the nail on the smoke drum, then shellac it and they would say that is the physiological event. When we used the Physiograph, it took only a half an hour of a three-hour period to prepare the animal to get physiological data, which was not restricted to mechanical events.
Nebeker:
So there was a real inertia in the community out there to accept the new machine.
Geddes:
They said that it was too complicated and the student couldn’t understand it. We said, “You don’t have to understand how your car works. You can drive it pretty well without this knowledge, can’t you?”
Nebeker:
That was an objection, that those people couldn’t understand the device itself.
Geddes:
Yes. Too complicated. Not in the good tradition of physiological education. When Grass came out with his polygraph, they said, “This is not a teaching unit; this is a research unit. The Physiograph is just a teaching unit not a scientific device.” I knew Grass well since my EEG days. And then, let’s see, there was another company that started to make polygraph. Gilson started to make them, Gilson Medical Electronics. He was an interesting person.
Nebeker:
What about the clinical side of this instrumentation. A lot of this must have had immediate applications?
Geddes:
Let me tell you something about the early days of ventricular defibrillation. The first human transchest defibrillation was in 1947. By about 1954 our students had all done ventricular defibrillation with a Physiograph. We had several calls in 1957 and 1958 from the local hospitals where we had former students. They would call and say, “Send us over the Physiograph defibrillator and the paddles. We have a patient in fibrillation. We’re doing cardiac compression. Hurry up. Send us the defibrillator.” So we sent the defibrillator over and they put the paddles on the heart and defibrillated.
Nebeker:
There were few companies out there producing any kind of defibrillator at that time?
Geddes:
As a matter of fact, it didn’t really start until 1952 with transchest defibrillation with a 700-volt 60 cycle alternating current defibrillator. Then Lown did it in 1962, ten years later, with a damped sine wave. And so, human defibrillation didn’t start until the early 1960s. Beck, the first to do human transchest defibrillation in 1947, had the same problem in Cleveland. He showed that you could defibrillate the heart if you exposed it and put electrodes across it. You plug the electrodes it into the power line, and pull it out in about one-halfsecond. People wouldn’t believe him. Prior to that, one had to cut open the chest, pump the heart by hand, put KCL in to depolarize the heart and keep pumping, and then pump calcium chloride in to re-polarize the heart. That procedure was used until the late ‘50s.
I used to demonstrate electrical defibrillation each year to all of the medical students, and the anesthesiologist from the local hospital would demonstrate chemical defibrillation. One had one chance with chemical defibrillation. If you didn’t get the doses right, you were out of business. Electrical defibrillation and patient monitoring came in late. It’s so natural now. Pacemakers didn’t come in until 1959 or 1960.
Nebeker:
It’s interesting that it started in the physiology lab and it sounds like people weren’t in a hurry to adopt defibrillation.
Geddes:
It wasn’t until our graduates got out and said, “I learned that in medical school. Why can’t I do it?”
Defibrillation research and defibrillator manufacturers
Nebeker:
We may move out of the chronology here. I know of your contributions to defibrillation. Just tell me how that research went.
Geddes:
There are three laws of defibrillation. We described two of them and John Schuder discovered the third.
Nebeker:
Who were you working with at that point?
Geddes:
- Audio File
- MP3 Audio
(406 - geddes - clip 2.mp3)
My mentor, Hebbel Hoff was always interested in defibrillation. At that time, it wasn’t known what was needed to defibrillate small and large hearts. We showed (and I can give you the references) that with directly applied electrodes, the current one needs and the energy needed increases with heart weight. The bigger the heart, the more energy and more current is needed. That’s with the direct heart defibrillation. We also showed that with closed-chest defibrillation, the bigger the subject, the more energy and the more current one needs with a given pulse duration. Some of our data points cost a thousand dollars; we even defibrillated horses. The tails of the largest animals defibrillated by us appear on the wall here. There is one camel and two horses. When I left Baylor, my technicians made this exhibit for me.
The first law of defibrillation is called the dose concept. The second law of defibrillation, which we discovered, was that defibrillation obeys the basic law of stimulation, the shorter the duration of the pulse, the higher the current, and the longer the duration the lower the current. The strength-duration curve is the fundamental law. It applies to defibrillation, and we published that in Medical/Biological Engineering & Computing. We first did it with capacitor discharges. Then we published the dose concept using damped sine waves in 1973 and 1974.
The third law was described by John Schuder at the University of Missouri. The law states, given a fixed pulse duration, the same pulse current intensity will not always defibrillate. There is a percent success versus shock strength curve, which is sigmoid shaped. Schuder has not received adequate credit for it, but nobody believed the dose concept either until the implanted defibrillator came along when it was necessary to know the minimum current (and energy) required for defibrillation so that the implant could be the smallest.
Nebeker:
What was the response of the medical community?
Geddes:
You see, cardiologists only saw adults. They knew they had difficulty defibrillating 200-pound subjects. But they could defibrillate most of the subjects with the defibrillators they had. Turn it up to the top and we defibrillate all. So, who is interested in the dose concept? That fight went on from 1974 for about the next eight or so years. It was only when they decided to make defibrillation efficient because they had to implant them that they began to know that big hearts are difficult to defibrillate. Small hearts are easy to defibrillate. It takes more energy for a big heart than for a small heart.
There are percent-success strength-duration curves for defibrillation; there is a family of them. One for 50% success, a little higher for 70%, a little higher for 90%, so that the strength-duration curve also applies.
Nebeker:
In reading about your work, there was another instance of some resistance, it seems, among cardiologists concerning your method for determining how good the contact of the electrodes was or the impedance measurement that you had done.
Geddes:
Yes. Everybody thought that it was energy that defibrillates because that is how the output of defibrillators were rated; i.e., stored energy in the capacitor, one-half CE2. However, there were some patients they could defibrillate and some they could not. It would depend upon how well the electrodes were applied because the electrode impedance and the size of the patient determines the current. We figured out that what you need to know is what the impedance is before the shock; so we developed a high-frequency measuring technique. It’s incorporated into the Hewlett Packard defibrillator. Other manufacturers use the method too. One passes a low intensity (35-kilohertz) current through the electrodes on the subject and measure the impedance to show the quality of electrode application. Hewlett Packard uses a series of lights: a red light for a bad application (high impedance) and a green light for a good application (low impedance). One applies the electrodes, get a green light, and then shock the subject.
Nebeker:
From what I was reading, it was not something that was quickly accepted.
Geddes:
No, it wasn’t. People just thought energy was the whole thing and didn’t think about current, which is what is needed to depolarize heart tissue. We had some knock down, drag out sessions. Most said, “Well, I can always defibrillate a big person or a little person with 350 joules.” That was knowledge gained from real experience. Well, for a big person one has to have the electrodes well-applied.
Nebeker:
What is the downside of using a very, very high current?
Geddes:
Myocardial depression and damage. If you use an excess shock, one will defibrillate, but the heart will be very slow to return to a strong beat and the first beats will be very weak. We conducted such damage studies. They were first done at Baylor and then finished here (Purdue). Excess shocks impair the myocardium enormously. You have to do CPR if you over-shock a heart.
Nebeker:
It sounds like the defibrillator manufacturers should be very interested in all these results.
Geddes:
They started to come around, but it took a little while. Every two years we would have a defibrillation conference here. Those meetings brought all the manufacturers, the researchers, and the cardiologists together. The first one was in 1975 and every two years after that. I think we had about five conferences altogether. Then we converted to a defibrillation and CPR conference. Then we stopped offering the conferences because everything was now in the industrial area. All the useful information was available and there was no more need for those conferences.
Nebeker:
Were you ever interested in the manufacturing side of defibrillation?
Geddes:
Never.
Nebeker:
Have you had close ties with any of the companies?
Geddes:
Yes. Several companies have funded our research. They would send us a defibrillator and ask us to test it or ask us to test the efficacy of one current waveform versus another waveform. Those studies started at Baylor in 1974. We defibrillated heavy pigs. Pigs are very difficult to defibrillate. Two-hundred-pound pigs are well insulated—lots of fat and it’s hard for the current to reach the heart. The question was, “Do you need a defibrillator with more than 400 joules?” So we did the study, and it turned out that, at that time, the defibrillators had a high internal resistance.
The manufacturers started to change that and put better inductors in with low resistance, and then the 400 joules was fine for the 100-kilogram subjects. But they couldn’t defibrillate 200-pound subjects, 100-kilogram subjects, with the existing defibrillators in 1974. One manufacturer developed a kilojoule, a 1000 joule defibrillator, and that is the defibrillator, the one we tested on the pigs. Then we found that when we got to thinking, that it’s current that defibrllates, not energy. So let’s get the current up by making the internal resistance very low. The high-energy defibrillator argument then disappeared.
Nebeker:
What has been the state of the art in defibrillation? Was a plateau reached?
Geddes:
An incremental jump occurred. Everybody thought that there must be an optimal waveform. The damped sine wave (underdamp and over damped), the square wave, and the trapezoidal wave; all had about the same efficacy.
John Schuder was interested in waveform efficacy. He investigated a positive wave followed by a negative wave. He did some studies that showed clearly that when one adds a negative tail of small amplitude, it was more effective. If one uses one with a long tail, it wasn’t as effective. People then became interested in optimizing the waveform, which is now called the biphasic waveform, which is a poor term; Schuder called a bidirectional wave, which is a correct term.
Then Baker and colleagues at Intermedics showed that the biphasic bidirectional waveform, with the second phase about a third of the first phase, defibrillated with a lot less stored energy and received a patent. This was designed for implanted defibrillators because it was desirable they wanted to make small implanted units. The implanted unit biphasic bidirectional waveform was born of the need to make a smaller and smaller implant. The Baker patent is the number one patent. Intermedics no longer exists.
John Schuder started the interest in waveform efficacy and then Baker showed the improvement in the efficacy. I published a paper last year reviewing all of this research. It is entitled Evolution of the Bidirectional Waveform. It gives credit to everybody who published research findings.
Nebeker:
This jump that you referred to occurred because of the interest in the implantable defibrillator?
Geddes:
Yes. The first ones were big units and were implanted in the abdomen. Now they’re sixty milliters in volume and implanted in the pectoral area.
Nebeker:
What about the standard hospital defibrillator? Has that been a stable technology?
Geddes:
Well, yes, it has. Most of them use damped sine waves. But now, the new defibrillators that are pre-applied, the ones that are in airplanes, use this biphasic or bidirectional waveform. And they can defibrillate with 150 to 200 joules. There are wearable defibrillators now. There are two companies making wearable defibrillators.
The old damped sine wave defibrillators are slowly being replaced by bidirectional (biphasic) wave units.
Nebeker:
Was that something that you looked into also, the efficacy?
Geddes:
Yes. We were convinced that we didn’t do the bidirectional waveform experiment quite right. It was just a little better. But Baker and colleagues showed that if you optimized that waveform, it’s a whole lot better. So we were close, but missed the boat.
Nebeker:
It really is the case that that particular waveform is clearly better than the two you mentioned?
Geddes:
Yes. I can give you a copy of my review paper if you want. Every paper that was in the literature, even the Russian papers, we analyzed. The paper is entitled "The Evolution of the Bidirectional Waveform". It was published in AAMI in Biomedical Instrumentation and Technology just last year.
Nebeker:
What about the role of patents in your own work in defibrillation?
Geddes:
Well, we’ve developed and got a patent for the method of defibrillation that requires sixty percent less energy over the conventional waveform. It uses two current pathways and two sequential pulses, and it is very efficient. But, it requires three or four electrodes. We patented it and one company liked it so much they bought the patent from Purdue. It was the first patent Purdue ever sold. But, that is the only defibrillator patent that I have. The company verified our results and has the patent on the shelf and they can dig that out anytime they want.
Nebeker:
This development of the portable defibrillator, the kind that a flight attendant can use, has that required some real advances in the technology?
Geddes:
No. Only advances in electrode application, electrode design, in capacitors that require less volume, in battery technology (because they are all battery operated) and the waveform. But it’s just a little improvement here and there. The big improvement is the waveform. The bi-directional waveform is the thing that makes it practical.
Patents and Purdue University policy
Nebeker:
Are there other things that you care to comment on in defibrillation? Other research that you might have done?
Geddes:
Yes. We have a patent and we’ve published on the control of ventricular rate automatically in atrial fibrillation. It hasn’t been licensed yet. It was just issued last year, but we published the paper. We can control ventricular rate in atrial fibrillation with an implanted device. It stimulates the left vagus nerve and it works very well. We can set the ventricular rate down to anything you want by programming it. But that’s way down the road because nobody believes that that can be done yet, although the principle it has been published.
Nebeker:
This is for an implantable atrial fibrillation device?
Geddes:
Exactly.
Nebeker:
Do you think there is an important need for that?
Geddes:
Well, more and more people are living longer and getting atrial fibrillation. So, the answer is yes. Some of them cannot have their ventricular rate controlled by drugs. That’s the patient niche, for our device. With drugs, the patient will often go back into atrial fibrillation frequently. The only thing you can do is ablate the atrioventricular node and put in a pacemaker. Our device does not do that; it detects the RR wave rate, which as the ventricular rate, decide what rate you want, and the device will stimulate the left vagus nerve to achieve that rate.
Nebeker:
What’s required here is for some manufacturer to believe there is a large enough market to make it worthwhile?
Geddes:
Exactly. And there are a lot of people interested, but nobody has yet said, “We will pay Purdue a royalty for a license to this patent.”
Incidentally, the university’s patent policy is very generous. I raised hell about it for ten years and they finally changed it. The university thought that all the intellectual property was owned by them—all your private thoughts were owned by Purdue. I pointed out to the Vice President and Treasurer, “You’re losing money, Fred.” He looked at me and said, “Why?” I said, “Faculty are taking their ideas out and patenting them on their own.” He gulped. I said, “There’s no incentive for them to patent through the university because there is no money coming back to them.” He said, “What do we do?” I said, “You change the rules; you divide the royalty and give the inventors one-third, you give the department or the laboratory of origin one-third, and the university takes one-third.”
Purdue implemented this policy and that has changed the complexion around here. It is a model. Students, secretaries, technicians, anybody can be an inventor if they contribute. But it gives the invention source slush money to do more inventing by having unobligated funds.
I have twenty-three patents now; however, about three of them are licensed. The university gets money and we get money. It is a win-win situation.
Nebeker:
They were all done through the university?
Geddes:
Yes, all of them.
Nebeker:
Why don’t people just continue to patent things themselves? I know there’s some cost involved, of course.
Geddes:
A patent can cost anywhere from $10,000 to $30,000 or $40,000. It’s a big bite. And the royalties you get from a patent are anywhere from five to six or seven percent. So it’s a real chunk of change from your pocket. The university pays for filing the patent. You get royalties when the patent is licensed. It is becoming a model for different universities.
We have a good office of technology commercialization, that goes out and sells licenses. There are few universities that have aggressive people in the patent licensing office. These are business people who know how to cut a deal, and they believe that a deal, even if it is a low royalty, is better than no deal. The person who turned it around was a professor of analytical chemistry. In this office, there are people with business backgrounds as well as engineers with MBA’s.
Other research at Baylor: NASA, electrical hazards, indirect blood pressure measurement, oscillometric method
Nebeker:
You were at Baylor from 1952 to 1974. What other lines of research did you embark on in those years?
Geddes:
One thing was that I was involved in NASA activities before there was a Manner Spacecraft Center. I was a consultant for the VSAF at Brooks AFB in San Antonio, TX for many years. In the early 1960’s, when I was at Baylor Medical College in Houston, NASA contacted me and invited me to be a consultant on physiological monitoring of astronauts before there was a suborbital flight. I along with other scientists (Pat Meehan and Col. Jim Henry) met with a few NASA people in a garage rented from Homco Oil Co. located at the intersection of Old Spansh Trail and Wayside streets in Houston. Then there was no Manned Spacecraft Center. We all discussed the important physiological events that we should measure and telemeter to earth from the astronauts.
From the outset it was obvious that it was desirable to telemeter the 4 vital signs (T, P, R, and BP), temperature, pulse rate, respiration rate and blood pressure. It turned out that the chimps on the sleds at Holloman AFB would not tolerate a rectal thermometer; they unceremoniously ejected it. The heart rate could be detected from the ECG. Respiration was detected by the cooling of a heated thermistor on the microphone in the helmet when the astronaut exhaled. In the first flights, indirect blood pressure was not obtained due to the cramped space. Accordingly, only ECG heart rate and respiratory rate were telemetered to the earth-bound monitoring stations. But there was a problem because the respiration signal was lost when the astronaut turned his head away from the microphone. At this point NASA contacted me and asked if I could devise a more reliable method of detecting respiration. On a Saturday afternoon at Baylor, I went into the lab, placed two electrodes across my chest at the xiphoid level and measured the 20 kHz impedance changes that occurred with respiration. The method was described later in Aerospace Medicine in 1962 and we used it in the medical student physiology laboratory; the method becomes known as impedance pneumography.
Soon it came time to implement the method for spacecraft and we gave all the information to the contractor to duplicate what we had done. They had difficulty and I sent my electronics expert, Marion Hinds (later professor of biology at Marion College in Muncie, IN.) to St. Louis to assist the contractor in building flight-hardened impedance pneumographs, which they did. However, before flight time, NASA did not have enough impedance pneumographs for the preflight areas; accordingly they borrowed several of our medical student lab units. Finally a spaceflight telemetered the ECG and impedance respiration to earth-bound monitoring stations.
Immediately, I realized that the ECG could be obtained from the same transthoracic electrodes used for respiration; this method, which was used in spaceflight was described in Aerospace Medicine in 1962. This method is still used in patient monitoring. Meanwhile, he problem of telemetering blood pressure was still unsolved for two reasons: 1) limited number of telemetry channels and 2) the need to create an efficient method of detecting the Korotkoff sounds, because at that time (the early Mercury, one-man spacecraft days) the auscultatory method was the only clinically accepted method, which required an upper-arm cuff and a stethoscope at the anterior bend of the elbow. Obviously this method was not applicable to an astronaut in a cramped space suit. It was obvious that what was needed was a cuff that incorporated a tiny microscope to detect the Korotkoff sounds. Accordingly, feasibility studies were performed with a piezoelectric crystal removed from a phonograph pickup. The crystal was about half the size of a portage stamp. A pocket, made of rubber, was glued to the rubber bladder about two thirds of the distance along the bladder toward the elbow and the crystal was inserted. Then the bladder was placed in the inelastic sleeve. With this arrangement, only the cuff need be applied to the upper arm of the astronaut.
Because of the small size of the piezoelement, I expected that the Korotkoff sounds would produce a small signal; however, the signals were large because the entire bladder in the cuff served to collect the sounds. In this way we had shown that a microphone placed under the cuff at its lower edge could be used to detect the Korotkoff sounds efficiently. A paper was published describing our results was published later in Medical of Biological Engineering in 1969. Soon another problem arose with use of our blood-pressure method, namely it required two telemetry channels, one for cuff pressure, the other for the Korotkoff sounds. At that time there was a limited number of telemetry channels. Therefore we electronically superimposed the Korotkoff sounds on the cuff-pressure signal; this technique was published by us earlier in the American Heart Journal in 1959.
Nebeker:
What other kinds of things were you involved in?
Geddes:
Electrical hazards also occupied me for a long time because there were a lot of hospital accidents. I was interested in what current and what body pathway was dangerous. We worked out data and it ended up in the FDA regulations for leakage current.
Nebeker:
What were the most common sorts of accidents?
Geddes:
Catheter-borne currents into the heart, into the body, producing ventricular fibrillation. The equipment that was connected to such catheters was not well designed at that time. It was an evolutionary problem. If the ground was taken off the device, then it would seek ground through the patient, so the leakage currents could be very high. That was one area that I spent a lot of time on and I published a book on it a couple of years ago, Handbook of Electrical Hazards and Accidents.
During my time at Baylor, I had always been interested in the measurement of direct and indirect blood pressure. I published two books on the direct and indirect measurement of blood pressure. We actually developed the oscillometric method, which is the standard method used now. We did the study that showed that when cuff pressure is decreased, the amplitude of cuff-pressure oscillations increased, reached a maximum, and then decreased. The maximum oscillation point signals mean pressure.
It was Maynard Ramsey at Critikon who said, “We have to get systolic and diastolic pressure from the cuff.” He developed algorithms from that amplitude spectrum to identify systolic and diastolic pressure.
Nebeker:
I was reading about that. That was 1969 when you and your grad student did that work.
Geddes:
Yes, with John Posey, a mechanical engineer who worked with me. Then he went to medical school. He is an anesthesiologist practicing in Houston now.
Nebeker:
You were getting the mean pressure from the cuff. Did you think at the time that this was something that ought to be useful to physicians?
Geddes:
Yes. The mean pressure is the perfusion pressure. It is the pressure that constantly acts to drive blood. If you have one pressure, that is the most important one. The peak and the minimum aren’t very important, systolic and diastolic. One wants a high mean pressure, because that is what is there all the time pushing blood.
Nebeker:
Before that, there was no easy way to get mean pressure measurements?
Geddes:
People then didn’t know what mean pressure was. Not that there was no easy way to measure it. They didn’t have a concept of perfusion pressure.
Nebeker:
They didn’t realize that this was a valuable measurement?
Geddes:
That’s right. Maynard Ramsey had real trouble with this because his first Dynamap only measured mean pressure. The user didn’t know what it meant.
Nebeker:
He had to add the systolic and diastolic.
Geddes:
That’s right.
Nebeker:
Did you and Posey think in 1969 that this was useful?
Geddes:
Yes. We thought that mean pressure was the most important pressure. We were a voice in the wilderness. We couldn’t convince anybody because they didn’t know what its significance was.
Nebeker:
Then, ten years later, Ramsey introduced the device, but, as you say, after adding the usual sorts of measurements that they were interested in.
Geddes:
That’s correct. The oscillometric method has some real value in the operating room, which is a noisy place. The method detects pulsations in the cuff pressure. Whereas with the conventional auscultating method with a stethoscope, one needs a silent environment and two things on the patient: a stethoscope and a cuff. With the oscillometric method only a cuff is needed and nothing else. One can operate in a noisy environment. Ramsey was smart enough to introduce it into the operating room with the anesthesiologists. That’s what made it take off.
Nebeker:
Is that widely used today?
Geddes:
Yes. You can go to a grocery store today and put your arm in a machine that uses the oscillometric method. The Omron Company, who is the leader in the use of the oscillometric method, has an annual sales of blood pressure measuring devices of many tens of millions of dollars. It has really taken off. I quickly got to know a lot about the economics of blood-pressure measurement.
Nebeker:
You and Posey didn’t patent this technique?
Geddes:
No. It was his Master’s thesis. It was just one of those academic exercises. I was curious and thought, “That must mean something.” It had been known since 1876 that there was this maximum oscillation, and people thought it was diastolic pressure; but it wasn’t. We decided to do an exteriorized artery experiment to find out what it means. That was the second area that I was interested in electrical hazards and blood pressure.
I was also interested in cardiac output measurement, and we developed a method using saline for measuring cardiac output. We patented it but we couldn’t get any interest in it.
I have always been interested in electrodes. Ever since McGill. I didn’t know what they were. What kind of a circuit did they produce? I was interested in electrodes ever since that time. In 1970 I wrote a book on electrodes, Electrodes and the Measurement of Bioelectric Events. That came at a time when disposable electrodes were just coming out. But there wasn’t that much interest and it went out of print very quickly.
I now give a course on electrodes in the spring and medical device accidents in the fall at Purdue. It is running now. I wrote books on both topics.
Progression of career at Baylor; transition to Purdue University
Nebeker:
Tell me a little about how things evolved at Baylor. Initially you were a grad student with Hoff and you completed your Ph.D. in 1959. What was your situation there?
Geddes:
I became an assistant professor, then an associate professor, and then a full professor of Physiology.
Nebeker:
Did you continue to work with Hoff?
Geddes:
Oh, yes. I taught medical physiology and taught the graduate students.
Nebeker:
On the research side?
Geddes:
Yes.
Nebeker:
You also worked with him in the laboratory?
Geddes:
- Audio File
- MP3 Audio
(406 - geddes - clip 3.mp3)
Yes. The polio epidemic was over by the late ‘50s or so. That was part of the rehabilitation, picking up loose ends. I went to work at Baylor full-time at that time. I was a professor of physiology. I also taught physiology at the Dental College, which was next door, and physiology in the Texas A&M Vet School, which was 90 miles away at College Station. That was a lot of fun, to go up two days a week and teach in one semester.
I taught physiology and I taught graduate students physiology and had graduate students doing research. I had a fur-lined rut at Baylor. It was just great. Then Hoff was going to retire and I was the heir for the headship of the department. The college was more interested in teaching medical students than they were in research because medical students brought in more money. The class went from 80 medical students when I arrived in 1952, to 220 when I left in 1974. Baylor decided to become a medical school to teach practitioners, and I was more in the research area. The writing was on the wall.
When Purdue started to knock on my door in 1972, I became slightly interested. Then I said, “How serious are you?” “Well, we’ll show you.” I said, “I’ve got a wife. I have two assistants who have wives who are professional people. One is a physician, Willis Tacker’s wife is a Ph.D. biochemist. My other associate, J. D. Bourland, has a Ph.D. in physiology with an EE degree. He has a wife who is a pediatric cardiologist. We have to relocate all these people if we come to Purdue.” And they said, “We will help you.” I kept putting up obstacles in front of Purdue.
One day, Tacker, Bourland, and I were at Purdue, and Tacker said, “They are going to remove every obstacle. We have to make a decision.” We made a decision to come in August of 1974. We all came, except my wife, who stayed a year in Houston to continue her teaching obligations at Texas Women’s University and Baylor Medical College. She came to Purdue in 1975 and became head of the School of Nursing in about 1980.
Medical instrumentation textbook
Nebeker:
Was it in 1968 that the first edition of your book with L. E. Baker on medical instrumentation was published?
Geddes:
I think it was. Here is the first edition, 1968.
Nebeker:
Would you tell me a little about how that book came to be?
Geddes:
That book came as a result of teaching medical students, residents, and interns, and the need to make devices for research. It also came as a result of the summer course “Classical Physiology With Modern Instrumentation.” There was just no way you could buy devices to make the measurements. Lee Baker was my graduate student. We decided that we would put this all down so people could learn how to make their own devices from a book. It’s really a measurement handbook.
Nebeker:
It’s become a real classic with three editions.
Geddes:
Yes. It is now about a thousand pages. I don’t think it will come into another edition because you can buy a lot of the things that you need now. Companies are around making transducers for anything and everything, and that was what that book was designed to do—to show you how to convert a physiological event into an electrical signal.
Nebeker:
So today it’s easy enough with off-the-shelf devices to make it unnecessary.
Geddes:
Yes. Chemical, mechanical, thermal, pressure—you can buy all of these things now. You couldn’t at that time. You had to create the devices.
Purdue University; starting Biomedical Engineering Center, gaining acceptance in EE field
Nebeker:
Tell me about the move here to Purdue. You started a Biomedical Engineering Center here.
Geddes:
Yes, We came Purdue in 1974, and we were in the basement of the EE building. I was the Showalter Distinguished Professor. It paid sixty-five percent of my salary. Purdue said, “You are going to get $200,000—one shot to start the Center; then you are on your own.” I had these three people to support: part of me, and Tacker and Bourland one hundred percent. So we decided what we were going to do. Tacker liked teaching; he is a good teacher and got an appointment teaching the medical students quarter time. We started to write grant applications like crazy. Before long we were bringing in $200,000 and ended up bringing in $2,000,000 a year in research funds. We just went wherever the buck was: NIH, NSF, industry, anywhere and everywhere. So the Center was a soft-money show.
Nebeker:
You had to raise a lot of money yourselves?
Geddes:
That’s correct. We created the Hillenbrand Biomedical Engineering Center and about a year ago it became the Biomedical Engineering Department. The university recognized that it is a legitimate academic pursuit; now there is a budget. George Wodicka is the head of the department. He is recruiting faculty and he has two faculty on board now.
I had an appointment in EE and Tacker had an appointment in the medical school. Charles Babbs came up as a new graduate with an M. D. and took his Ph.D. at Purdue, and we supported him in research.
Nebeker:
Were you regarded as somewhat odd in the EE department at that time?
Geddes:
To say the least. One professor said, “You mean to tell me that frogs are part of a EE curriculum?”
Nebeker:
Were you using animals in your research?
Geddes:
Yes. We had a physiology lab. I will take you around and show you what we have here. We have a dog lab down in the basement in EE. They just didn’t know what the to do with us. We hired an animal tech and he is still with us. We started a course called “Problems in the Measurement of Physiological Events.” It’s a miniature summer course from Baylor. It has been running since 1975 every spring and it enrolls about 20 students each year. Experimental physiology is what it is—dirty-finger physiology and biomedical measurements.
Nebeker:
What about the other faculty members? Were there any in EE or elsewhere that were interested?
Geddes:
Yes. All the schools at Purdue have what are called areas. In EE there is a computer area, there’s a robotics area, and there’s a communications area and a biomedical engineering area. Then there were three EE faculty members who are interested in some aspect of using electrical engineering to solve biomedical problems. The first one was the recording of electrical activity of cockroaches exposed to insecticides, because they were neurotoxic insecticides.
At that time there were also image processors and some very good image processing researchers. Kak wrote the algorithms for a new processing for CAT scanners. But, he didn’t get the recognition because he was a little late in describing his work. Then there was another professor who was interested in control theory, i.e. the control systems of the body and how the blood pressure was regulated. There was another professor who was an electronics type, and he was building a disposable fiber optic pressure transducers. Now he is about to retire.
There were signal processors who developed algorithms for ECG analyses that led to a company named Vetronics. We were systems people and kind of flamboyant, mavericks. We developed a machine shop, a physiology lab, and an electronics shop along with a radiology suite and a sterile surgery.
Graduate students at Purdue; pedagogy and student accomplishments
Nebeker:
You managed to attract graduate students here?
Geddes:
Oh, yes. At that time with no department we had many graduate students, and they would get their degrees from their parent department, like EE, ME, ChE, Vet Medicine, Psychology etc. They would do their research here and we would support them and their research with our research funds. They would get the degree from the parent department. The arrangement was that there would be at least one and maybe two members of the parent department, ourselves, and anybody else the student wanted on the graduate committee.
Nebeker:
I have a list of your Master’s and Ph.D. students, and it is a formidable list. Could you pick out three or four former students and comment on their work?
Geddes:
Let me start with the first one. John Pearce came from Clemson University with a Bachelor’s degree in Mechanical Engineering. He had worked on sleep surfaces, fluidic beds, to distribute the body pressure evenly so that there were no high pressure points to produce bedsores. He came into the lab one day and said, “I am John Pearce and I want to work in electrosurgery.” I said, “John, we’re not doing any work in electrosurgery.” “It doesn’t matter,” he said. “I would like to work somehow in electrosurgery.”
I got to thinking about, “What are the problems in electrosurgery?” We went to industry and got a little money, and he started. He entered EE as an MS student. We acquired some money and started to design electrosurgical electrodes. With his background in mechanical engineering and in electrical engineering, he modeled the thermal distribution in a phantom material using its electrical and mechanical properties for an electrode on the skin surface. He showed the high current density at the perimeter and the high temperature under on the perimeter under the electrode perimeter. That impressed me very much.
While we were getting industrial support, we went to the FDA and said, “You ought to know about such electrodes because you have to write performance standards for such electrodes.” They said, “Yes.” I said, “I have a grant application in NIH and they won’t fund it.” They said, “They won’t fund it?” I said, “Yes.” They said, “It’s good stuff.” I said, “Is there any way the FDA can get together with NIH?” And they said, “We think so.” So NIH and FDA got together and they funded us. That got John Pearce going in thermal imaging. His Ph.D. thesis is the basis of the FDA standards for dispersive electrodes for electrosurgery.
He received an MS in ME while he was here. John is a real eager go-go person; nothing is too difficult. He was about to graduate and Purdue has a policy that it will not hire its own graduates for faculty. So, he had to leave and went to the University of Texas in Austin, and before a year was out, he had a Presidential Young Investigator Award. He is now a titled full professor at Austin in Electrical and Biomedical Engineering. He pioneered things that just hadn’t been done, putting the electrical, the mechanical, and the thermal together. That’s an excellent accomplishment for a graduate student.
Nebeker:
It’s good that you didn’t turn him away when he said he just wanted to do work on electrosurgery.
Geddes:
- Audio File
- MP3 Audio
(406 - geddes - clip 4.mp3)
If somebody wants to do something, I’ll help them. If they want me to do something for them, they are going to wait a long time. I’ll help anybody who has an inclination to do something. Pearce was one of the first PhD graduate students and there have been quite a few others since.
The most recent one, is Becky (Rowe) Roeder. If you hold her still, she will bore a hole in the ground. She has a Bachelor’s in Mechanical Engineering, an MS in physiology, and she is now a Ph.D. student in Biomedical Engineering. She has done all kinds of research for me and has an aptitude for solving problems. In the last few months we have developed a new method for measuring blood pressure in the limbs of neonatal and premature infants. At present, indirect blood pressure cannot be measured accurately in these subjects. She has developed vascular grafts and we have implanted them, and the vascular grafts remodel. They are made from small intestines.
She is now working on a method for detecting the cardiac output for an implanted converter-defibrillator. The problem is that if the heart goes into ventricular tachycardia, a defibrillating shock is delivered to arrest the tachycardia. It takes about half the energy to stop a tachycardia as compared to arresting fibrillation. What you need to know is that they now only use the ECG to trigger the shock, and that doesn’t tell you anything about cardiac pumping. We have developed a new method for detecting the amount of pumping during a tachycardia and fibrillation event. We have filed an invention disclosure and our device will be the next generation of implanted cardioverter defibrillator because it is sensitive and only shocks when the cardiac output goes below a certain programmed value and the electrical (ECG) rate is an above certain value. Becky has a bright future ahead of her.
Now, our students have gone all over the world. For example, one of my students, John DeFord, is the chief Executive Officer for Cook Incorporated. He is in charge of forty Cook companies. He graduated about ten years ago with a Ph.D. in EE. He was the first person to pace the heart with pulsed ultrasound. Then he developed a selective hyperthermia system to kill malignant brain tumors and spare the adjacent normal tissue. His thesis founded a new company to build these devices to heat the tumor and spare the surrounding normal tissues.
Many of my graduates are in the medical device industry. They are all chief engineers or VPs. The thing that we do well here is make the students join theory and practice. They have got to get out in the lab and use the theory and face up to its operation in living beings, either animals or themselves.
Nebeker:
So, there has to be some empirical data that validates the analysis or modeling or whatever.
Geddes:
We want to turn out people who are useful to society and in particular, useful to industry. We developed a pressure-sensing system for measuring the pressure at 1500 points below the supine body. A company came to us and said, “We have a new sleep surface. We think it is better than anybody else’s but we don’t know how to evaluate it.” We replied “well, you want to determine the pressure distribution under the body. We developed a system that uses a row of aluminum ribbons and there was sponge rubber between and another row of aluminum ribbons at right angles. Each of these intersection points is a capacitive pressure transducer. They measure the capacitance as the pressure squeezes these two ribbons together. The pressure is displayed on a computer screen.
It writes out a contour map on the monitor. You can see here is the pressure distribution map; here is the head, the shoulder blades, the sacrum, the buttocks, the thighs, the calves, and the heels. We measured the pressure under the sponsor’s sleep surface, and measured the competitor’s sleep surface, and the sponsor’s wasn’t any better. They took a gulp and redesigned their sleep surface. What they are using this pressure-mapper for now is as an advertising device. They converted the contour map to a color map, which, is displayed in the sales room, and they can show that their sleep surface has been scientifically designed. One can put the hand on the mat and see the color. It fascinates the potential consumer.
Nebeker:
So, it’s a good marketing tool.
Geddes:
It’s an excellent tool now, yes. Not a research tool now.
Historical publications; importance of historical awareness for engineers
Nebeker:
I was looking through your nearly eight hundred publications, by my count. It is a little difficult to classify. Something like sixty-five of them are historical papers or books. I know that started very early with you.
Geddes:
It started with my mentor, Hoff. He was a medical historian. He knew why everything was the way it is. He knew what a cubit was. He knew the origin of millimeters of mercury for pressure. He knew just about every thing. He had written lots and lots of papers on history, and he stimulated my interest in history. For example, I wanted to know how Ohm did it when there were no voltmeters and no ammeters. There were galvanometers, but they were uncalibrated. I become interested in Ohm’s work.
Nebeker:
You wrote some papers with Hoff, I noticed.
Geddes:
Yes, quite a few with Hoff.
Nebeker:
You continued over the years to do historical work?
Geddes:
Yes. The fun one was the Galvani-Volta controversy. Galvani thought that there was animal electricity.
Nebeker:
A new type of electricity?
Geddes:
And then Volta said, No. This is due to dissimilar metals and the electrolyte produces electricity.I had a military background and that fascinated Hebbel Hoff. We wrote some papers on ballistics, and the ballistic techniques were used to measure the nerve impulse velocity.
Then I began to wonder about the creation of short-duration pulses to measure the excitability of nerves to get the strength-duration curve, which is a plot of threshold current versus pulse duration. Well, a man in 1880 (or thereabouts) generated pulses of a millisecond and a tenth of a millisecond in duration. There were no vacuum tubes. How did he do that?
He had stretched wires between posts and he could choose the separation between the wires. The cutting of the first wire with a bullet started the current to flow and stimulate the tissue, and cutting the second wire stopped the current. The bullet went into a ballistic pendulum, which was deflected. The amount of deflection of the pendulum told the velocity of the bullet, and the distance between the wires identified the duration of the pulse of current.
Nebeker:
Amazing.
Geddes:
Yes. Isn’t that incredible? I was always amazed at how those scientists just used brain power to substitute for a lack of technology.
Nebeker:
At the IEEE History Center, our mission is to cultivate the history of electrical technologies. We think that is very important because engineers should be proud of the heritage that they have.
Geddes:
And they don’t know it, by and large.
Nebeker:
Typically, young people, students, have no idea about the past of engineering.
Geddes:
Yes, and what a struggle it was to get the knowledge. Students just accept it as ordinary and obvious.
Nebeker:
That’s right. I think that is justification enough for learning the history, that you are part of a long tradition and you should know the people and the great names who preceded you, especially when those names have become a unit or some technique that is named after that person. Do you think that the study of history is useful in other ways, such as understanding how instruments work or even getting ideas about how one might approach current problems?
Geddes:
Yes. Let me just divert you a second and tell you why I am writing this series of historical articles in the EMBS magazine in the Retrospectroscope. I think it lends a great deal of credibility to a lecturer when he is lecturing on a subject and he introduces it with the history. Because it shows the continuity and that is the thing that is missing in modern teaching. They just don’t tell you where it all came from.
Nebeker:
You were saying that it is very important as a teacher to provide historical background.
Geddes:
Yes. I think it is important because by knowing that, down the road the student will perhaps be able to make the next leap from the knowledge that he or she has now. It gives them the thought that it is an evolutionary process. It is not a sudden discovery; it is an evolution. For every discovery, there is a little background and there is going to be a future. We are not at the end now.
Nebeker:
You present this time sequence up to the present, rather than state of the art and end of story.
Geddes:
That is not the way I lecture. For example, I give a lecture on the pacemaker. I made a sketch of the first cardiac pacing experiment. It was done in 1872 by Steiner in Germany. His pacemaker consisted of a battery and a metronome, which was the switch. He stuck a needle in the heart, and an electrode on the chest, and he noticed the needle moving as the heart beat. Now, why did he do that? That’s important. Because at that time, chloroform was the anesthetic and chloroform stops the heart in some subjects as one of its side effects. It is a great anesthetic, but there is temporary cardiac arrest.
Steiner thought he could stimulate the heart. He gave the anesthetic to the point of cardiac arrest. Then he started to stimulate the heart with his metronome. He did eight horses, seven rabbits, some dogs, some sheep, and one human. It failed in the one human, but it worked in all of the others. Now, here is the beginning of cardiac pacemaking. Modern pacemaking started in 1959 with Furman; but there was a long history before that. There were some closed chest pacing with the inductorium. The modern concept is around because the technology is now available to do it easily. But the knowledge was known more than a century ago. One ought to know the historical background.
Nebeker:
Occasionally, an earlier approach that didn’t result in anything useful might become feasible when new technology arrives.
Geddes:
That’s exactly the point. New technology is around and one can do things now that were very difficult to do previously. The knowledge was around, but the execution was very difficult.
So, I always start my lectures with the history and what was done and why it was done. To just say what was done is not enough. One has to get into the mind of the person who did it to find out why he did it. I think that stimulates the kids a lot more than just hearing that the Battle of Hastings was in 1066. “The Battle of Hastings was fought because…” is the right way to approach it. I used to not think that way. When I was taught history in school, one had to remember the dates of the reigns of all the kings of England and the dates of all the battles. Not why they got there, and why they didn’t and why they died. One had to have a mental laundry list, and that to me was unsatisfactory history. Then I was exposed to Hebbel Hoff and he always gave the rationale for the history, and that fascinated me.
Nebeker:
I am very pleased that in some of your books that there are historical introductions or addenda.
Geddes:
Yes, a postscript here or there.
IEEE Engineering in Medicine and Biology Society
Nebeker:
It’s very interesting. I also want to ask you about the IEEE Engineering in Medicine and Biology Society with which you have been associated for many, many years now. If you would just say a little bit about how that has evolved over the years. You said that you started attending the meetings in the early ‘50s.
Geddes:
Even the late ‘40s.
Nebeker:
In the late ‘40s, you started attending that annual meeting?
Geddes:
Yes. At these IRE meetings there was a fellow by the name of Jan Nyboer. You probably haven’t ever encountered that name. He was one of the first to demonstrate the value of using impedance to measure physiological events. His original summary of the field is in the 1947 edition of Medical Physics. Are you familiar with that series, Medical Physics?
Nebeker:
Yes.
Geddes:
Then he and Herman Schwan got into discussions at these meetings, Herman being the scientist, Nyboer was a physician and he was using tetrapolar electrodes to eliminate the electrode impedance. He was measuring respiration and cardiac impulses. Herman Schwann was all upset that Nyboer didn’t know the resistivity of the tissue, and their distributions. It was going on and on and on.
So, those meetings were quite controversial in those days because there were people on one side who wanted to make measurements and didn’t have the knowledge of the proper way to do it, and there were people on the other side who were good engineers and knew how to do it, but didn’t know the meaning of the measurement. They got to be rather interesting meetings from time to time.
But they were a forum, which started to develop communication. We were all alone in those days. I was in Montreal at McGill doing my thing and I didn’t know there was one by the name of Herman Schwan at the Moore School of Electrical Engineering doing his thing. I didn’t know there were others doing interesting things like I was doing. Nyboer was in Detroit. We got to know that there were other people doing things, and that was the real value of these meetings. One could look forward to a meeting to meet people doing things whether you liked them or not, whether they were doing good work or bad. One learned what was going on, so that was the fun of these meetings.
Nebeker:
You joined the professional group on Medical Electronics as it was called?
Geddes:
Yes. I started to subscribe to the journal. Otto Schmitt was big in those days. He was very vocal for the field, and he was a very practical person, too. He did very good theoretical things. So, the meeting provided a chance to see beyond your own area.
Vladimir Zworykin
Nebeker:
Did you ever encounter Vladimir Zworykin?
Geddes:
Yes. I met Vladimir Zworykin and I knew him very well. As a matter of fact, he has a plaque in the Purdue EE building and his family gives money to the university for a fellowship. He was visiting when I met him in the late 1940s or early 1950s. He was working with R. Stuart Mac Kay and making endoradiosondes—swallowable pill-sized telemeters. Zworykin was very big in that area and was even bigger in television.
Nebeker:
He was one of the giants of television development. But, in the last period of his life he was most interested in medical electronics.
Geddes:
Exactly. He pioneered the radio pill, as it’s called. I met him; he was a very interesting person. He was a Russian, and got his training in Russia from Nipkow. You probably know the Nipkow disk, the first flying spot scanned. Do you know where the Nipkow disk is?
Nebeker:
No.
Geddes:
It’s in Japan. I found it in a museum in Japan. It’s a big ten-foot or eight-foot disk with perimeter holes in it. Of course, Zworkyn’s contribution was seeing that this mechanical flying spot scanner could be made into an electronic device. Then he went from that point on.
I met him again in Japan at the Tokyo Prince Hotel when he was talking about his endoradiosondes. It was an international conference. I guess it was the IFMBE (International Federation of Medical and Biological Engineers). He did things that are even hard to do now—make little pill transmitters and the batteries and the transducers for them.
Nebeker:
That particular device has never been that useful, is that right?
Geddes:
It’s coming back. The gastroenterologists are now interested in measuring the pH as the pill goes through the GI tract. It has to have a clinical niche to be used.
Nebeker:
So fifty years later, we have history coming back on us.
Geddes:
They are measuring the pH along the esophagus now with a catheter electrode. The stomach is the site of most interest. But, that is only part of the story. They want to know where the sensor is, and that’s the missing link, so one needs some sort of a locating means. One can telemeter the pH. Scientists are working on a locating means.
Growth of biomedical engineering field
Nebeker:
Over the years, of course, the professional group on electronics has grown enormously from dozens of people in the very first meetings to thousands now.
Geddes:
Yes, it was just a little handful like twenty or thirty people.
Nebeker:
The number of publications has expanded enormously. Do you find that the field is getting very fragmented?
Geddes:
I don’t know that it is getting fragmented. It has changed. The transactions on biomedical engineering are becoming a little more theoretical and modeling than they used to be. The trouble is that doing experiments is expensive. It is easier to sit at the computer and put data in and model. It is expensive to take those data and subject them to the real world animal or human test. So that is a change that I am not particularly happy to see because I like to see theory and practice joined.
There are two kinds of models. One can take a physiological event, measure it, then put it into a model, and then check to see if the model reproduces what you put in. The other way is to create a hypothesis, create a model, and test the model with the reality by experiment. The latter is what I prefer: get a hypothesis, enter the data, and then find out if your hypothesis is right by the experiment. Then you modify conditions and discover if the model will allow you to make predictions; then you can check the predictions.
Nebeker:
Is there anything that I haven’t asked about that you would like to comment on? There will be a chance later to add anything that you would like.
Mentors and collaborators
Geddes:
The only thing that I can say is that I have been blessed with good mentors at McGill. There were people there who just would not accept defeat. It was just wonderful to be around people like that. When I went to Baylor, there was no department of surgery. DeBakey was in the department of medicine. To see him put that together and to create his vascular grafts, knit them himself, he just wouldn’t stop, he was an inspiration as was Hoff. And, being in the Texas environment, then with two hundred thousand people in Houston, it grew tremendously and had an atmosphere of progress. I got a chance to meet all kinds of people. They were real mountain climbers.
So I was really blessed with not only academic excellence but with being in front of people who just got in and did it. When they made a decision, it’s going to happen. So, it was just wonderful to see these people operate and overcome all kinds of difficulties.
Nebeker:
Thank you very much.