This article was initially written as part of the IEEE STARS program.
Citation
As a result of the pioneering work of many scientists, engineers, and doctors, the fully implantable pacemaker was invented and developed in the mid 20th century. This is a medical device that uses a power supply (battery) and electronics to generate electrical impulses to keep a human heart pumping when the internal electrical timekeeper of that heart has failed. By the end of that century, some 100,000 artificial pacemakers were being implanted annually worldwide into patients, almost all of whom benefited from extended and enhanced lives.
Introduction
An interest in the interaction between living organisms and electricity dates back to the beginnings of electrical science. Luigi Galvani’s anatomical experiments in the late 18th century led him to observe that an electric spark could cause the muscles of dissected frog to twitch. The growing knowledge of the human body led to experimentation on a wide range of electrotherapies by pioneering scientists and physicians, and also by quacks. These techniques employed both direct current and static electricity. It was already known that the heart responds to mechanical blows to the chest with a fist, a technique now known as percussive pacing. It soon became clear that the heart was an organ especially sensitive to electricity as well.
As early as 1788, attempts were made to treat irregular heartbeats with an electric shock, and in 1872 T. Greene in England published an important but sometimes overlooked paper showing that electric shock could restart a stopped heart. By 1878 Munich surgeon Wilhelm von Ziemssen discovered that periodic pulses of DC current applied to the chest could cause the heart to accelerate until its beat coincided with the external stimulus. John Alexander McWilliam then proposed in 1889 that small, regular electric pulses could be used to treat conditions where the heart was beating irregularly or at the wrong rate. In 1899 he published key experiments demonstrating his thesis that regular heart rhythm could be evoked by applying regular impulses.
Impact of Commercial Electric Power Distribution
With the spread of commercial and domestic electric power and its danger in the late 19th century, researchers began to study why and how electric shocks could be fatal. They came to realize that it was the result of heart failure. Jean Louis Prevost and Frederic Battelli in Geneva and Richard Hope Cunningham in the United States then discovered that rapid application of a second large shock could sometimes restore the heartbeat and return the victim to life via what is now known to be defibrillation cardioversion. One problem was that often the heart would stop again. Physicist Edgar H. Booth and surgeon Mark C. Lidwell in Sidney, Australia developed an AC-powered apparatus which could deliver large shocks to the heart at regular intervals. In 1928 they used it for ten minutes on a stillborn infant, who subsequently recovered. It became clear, however, that there were two closely related but separate challenges: 1) defibrillation, that is, synchronizing a quivering, non pumping heart, and ultimately being able to artificially stop and start a heart during surgery; and 2) correcting the heart rate of a heart that was not stopped, but not functioning properly either.
Albert Salisbury Hyman, a New York cardiologist, took up the second challenge. In 1932 he described an electromechanical instrument of his own invention that was powered by a spring-wound hand-cranked motor and delivered, by means of a needle, a regular small pulse to the right atrial area of the sinus node where the heart’s natural pacemaker is located. Hyman coined the term "artificial pacemaker" to describe it, and he conducted animal experiments and perhaps one clinical trial, but was unable to interest manufacturers. The medical establishment resisted his technique because of the difficulty and danger of placing a needle directly into the heart. He did eventually manage to produce a few copies of the machine, dubbed the “Hymanotor,” but its medical impact was small.
Hyman’s partial success led a team from the University of Toronto to take up the challenge of pacemaking. In 1950 cardiothoracic surgeons John C. Callaghan and Wilfred Gordon Bigelow of the University of Toronto and the Toronto General Hospital persuaded the Canadian National Research Council to assign an engineer, John A. Hopps, to work on the problem. The argument was made that there was a risk to national security with soldiers experiencing slowing of the heart upon exposure to extreme temperatures. The team improved on Hyman’s work by developing an AC-powered device using vacuum-tube technology to provide pacing to the heart from outside the body, and they successfully demonstrated it on canine subjects.
This work in turn inspired Paul Maurice Zoll, a Boston cardiologist who had been working on defibrillation. He realized that some of the improvements made by the Toronto team could be used to help his own defibrillation work, but he also saw how the knowledge he had been acquiring could be applied to pacemaking. He built an improved device and, in 1952, he kept alive a 65-year-old man with recurrent cardiac arrest by external stimulation for 52 hours. The patient survived for six months. Zoll’s seminal publication in the New England Journal of Medicine led to the recognition of pacemaking as a fruitful area for future research.
The two main drawbacks of the pacemakers made by the Toronto group and by Zoll was their size, and the problem of delivering the shock directly to the heart. Although they were portable in the sense that they could be wheeled into the patient’s room—unlike, for example, x-ray machines at that time where the patient had to be brought to the device—these early pacemakers were large and cumbersome, and the patient had to be constrained. Another major problem was the power source. Using AC because batteries could not effectively power such large instruments, so the devices required the patient to be plugged into the wall.
The second problem was solved in 1959 when Seymour Furman, working at Montefiore Hospital in the Bronx, New York pioneered a technique to keep the heart going during surgery by connecting the pacemaker to the right ventricle with a lead passed through a vein, rather than with a needle. This technique is today called transvenous pacing, as opposed to transcutaneous pacing when the shocks are delivered through the chest. (When the heart is actually exposed, as in open-heart surgery, any pacing done is called epicardial pacing because the leads are placed on the epicardial surface of the heart.) However, the size issue continued to limit the effectiveness of pacing for ambulatory patients.
Solid-State Solutions
Late in 1957 Dr. C. Walton Lillehei, a pioneer in open-heart surgery at the University of Minnesota, asked Earl E. Bakken, co-founder of Medtronic, Inc. (a small, local medical instrumentation firm), if it would be possible to develop a battery-operated pacemaker. Bakken realized that the recently developed solid-state electronics were the answer. Within four weeks he had produced a prototype that could be worn on a belt, with the leads running up to the chest. By having the leads penetrate the chest, there was no problem with the patient being ambulatory, and even smaller batteries could be used. Almost immediately Lillehei used it for treating children who had developed heart block after surgery, and he published his results in a major medical journal. This wearable, transistorized unit was produced commercially as the Medtronic 5800 pacemaker. Initially limited to a few hundred units, this pacemaker liberated patients from their power-cord tethers, demonstrating once and for all the safety and effectiveness of pacemaking as a medical technology. As a result, Medtronic became well established as a manufacturer of medical devices and perhaps the industry leader in external pacemakers.
The next significant challenge was to make a device that was fully implantable. If the heart could be paced from inside, it would reduce the danger of infection and free the patient not just from the bed but from the hospital. In order to achieve full implantability, however, it would require a device that was extremely light and that employed a battery that was sufficiently small yet long-lasting. In addition, the electrical leads would have to be able to accommodate substantial current while being contained completely within the body and not harming any tissue. A number of techniques were tried. In 1958 engineer Rune Elmqvist and surgeon Åke Senning at the Karolinska University Hospital in Solna, outside Stockholm, developed a device using rechargeable batteries that could be implanted in a patient and charged externally with an induction coil. Although the device failed after only three hours, many historians consider the patient, Arne Larsson, to be the first human to have a fully implanted pacemaker. Larsson also received the world's second fully implanted pacemaker within 24 hours of his first procedure. Arne went on to have a total of 22 pacemakers and 26 operations (some of which were to replace leads). Over the next two years a series of trials eventually resulted in a patient living nine months. Medical engineering had passed another milestone, but a truly satisfactory implantable pacemaker was not yet available.
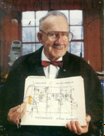
That availability occurred following clinical trials beginning on 15 April 1960 when William C. Chardack, a surgeon at the Veterans Administration hospital in Buffalo, New York, assisted by Andrew Gage, implanted devices into the chest cavities of a series of ten patients with heart problems caused by failures of their hearts’ electrical systems. The inventor of the device, local engineer Wilson Greatbatch, had heard about Bakken’s work, and thought he could solve the battery problem. He eventually convinced Chardack to work with him. The device, for which Greatbatch obtained a patent in1962, used a two-transistor, transformer-coupled oscillating circuit powered by a mercury battery. The patients, who formerly would have died within weeks under any known treatment, lived for another eighteen months to thirty years. Since Earl Bakken already had in place the infrastructure to produce and distribute pacemakers, and because Chardack and Lillehei were friends, Greatbatch licensed his invention to Medtronic. Greatbatch continued to design and patent improvements in pacemakers for Medtronic until 1972. One of his last achievements was the development of a five-year lithium battery, which became the industry standard for use in pacemakers. At the same time, Cardiac Pacemakers, Inc. also of Minneapolis (it was founded by former Medtronic engineer Manny Villafana) pioneered the technique for hermetically sealing the pacemaker in a titanium alloy case.
The technique was becoming widespread enough in the early 1970s that in 1974 the U.S. Food and Drug Administration commissioned a study to report on its safety and effectiveness. By 1976 manufacturers had to provide appropriate documentation and eventually clinical studies to receive FDA approval for commercial release of their devices.
Recent Developments
That FDA-commissioned report, known as the Bilitch Report, finally issued in 1994. The report emphasized the outstanding success of pacemakers, and remarked on the improvements that had been made just in the 20 years since the study was begun. The continuous improvements in the cardiac pacemaker were related to the great advances in the 1970s, 1980s, and 1990s in other areas of engineering, such as power, materials, and electronic devices. Specifically, there have been significant advances in battery life, biologically neutral packaging, and, especially, microprocessor-based control of the rate and type of pacing. Beginning with Bakken’s model, the pace could be adjusted, but the heart had to be monitored separately. Already in 1973, Cordis Corporation released the Omni series, the first externally programmable implantable pacemaker. By 1982 Dr. Anthony Rickards of the National Heart Hospital in London was able to introduce the first physiologically adaptive pacemaker—that is, he invented a pacemaker that used sensor technology and a microprocessor to automatically adapt the heart rate to the body’s demands. In 1988 Raul Chirife improved upon this work by implanting the first responsive pacemaker to utilize a hemodynamic sensor (a device that can sense actual blood flow). Although that device was never brought to the commercial market, the technology continued to advance, and the use of pacemakers continued to grow dramatically during the period. Therefore, the first official guidelines for the use of pacemakers were published in 1998 by a joint taskforce of the North American Society of Pacing and Electrophysiology (NASPE) and the British Pacing and Electrophysiology Group (BPEG).
The years since the Bilitch report were to see as least as many advances as the years during its preparation. Through the 1990s, pacing had consisted of two modes that are still used today. The simplest type is single chamber, when the electrode is planted in the left ventricle. In the other technique, dual chamber, an electrode is placed in each ventricle. In 2005, however, a third technique, biventricular pacing, also known as Biventricular pacing for Cardiac Resynchronization Therapy (CRT), was introduced. Here, two pacing electrodes are placed on opposite sides of the same ventricle to promote synchronous contraction to improve pumping efficiency, allowing for better control of the heart rhythm. There are advantages and disadvantages to each of the two original modes and the new mode as well. Inappropriate pacing of the right ventricle can lead to heart failure and increased atrial fibrillation. Dual chamber pacing can reduce the need for right ventricular pacing, but dual chamber pacing can cause pacemaker mediated tachycardia in which the pacemaker itself creates a conduction path for rapid heartbeat (though reprogramming can usually remedy this situation). Biventricular pacing may not deal with certain conditions impacting both ventricles.
However, thanks to the small size and power requirements of modern electronics, all of these modes can be combined in one device, and sensors and control systems can make the pacemaker rate responsive to changing demand for blood flow. The various types of sensors now available can detect not just acceleration and blood pressure, but also the concentrations of oxygen, carbon dioxide, ATP, and adrenaline in the bloodstream. The devices can actually record electrograms. (Technically, electrograms are recordings of the electrical activity of the heart from a lead inside the heart, while the more familiar electrocardiograms are recordings of the electrical activity of the heart from the body surface.) The electrograms can be analyzed in real time to sense the need for an adjustment in heart rate. The sensor information is used by control algorithms to make the artificially paced heart mimic a naturally paced heart in every respect.
As a result, the state of the art includes technology for temporary pacing during surgery and acute care, as well as technology for implanted permanent pacing. Such therapy is used for both bradycardia (slow heartbeat) and tachycardia (rapid heartbeat). Tachycardia is treated with more sophisticated pacing technology and, in the case of fibrillation, with a modern electrotherapy device called the cardioverter-defibrillator or implantable ICD.
At the same time, these advances allow the implanted pacemaker to double as a device that can detect, store, and report continuous heart electrical and mechanical activity, thereby replacing temporary monitoring devices such as a Holter monitor. Even while treating the patient, the device is supplying valuable medical feedback to help determine the optimal therapy continually.
The technological advances in the fully implantable artificial pacemaker have been matched by expanding penetration into society. By the end of the 20th century, more than 200,000 artificial pacemakers were being implanted annually worldwide, by conservative estimates. This significant technological achievement has resulted in millions of patients benefiting from an extended life span and an improved quality of life.
This success also creates inertia against the implementation of innovative features since a substantial amount of training needs to be done before an approved feature can be released: in recent years only one new feature every two years on average. There are other therapies--electrical, pharmacological, and surgical--for cardiac problems, and there is still more to learn about cardiac physiology. The trend is to make artificial pacemaker devices smaller and more natural rather than have them last longer, with the current average lifespan at seven to ten years. Competing developing technologies like artificial hearts and tissue engineering are also a consideration for the pacemaker industry. Whatever its future, numerous surveys from the Bilitch report up until today have consistently placed cardiac pacing among the top ten biomedical technologies for high-quality life extension. The artificial cardiac pacemaker is truly a significant technological achievement of engineers, scientists, and doctors that has benefited humanity.
Acknowledgements
The authors thank members of the STARS Editorial Board and the History Center staff and the outside reviewers for their feedback, and also the others who provided review and constructive criticism of various stages of this article, with special thanks to David Geselowitz, Dorin Panescu, Max Valentinuzzi, and Alex Zapolansky.
Timeline
- 1788, First attempts to treat irregular heartbeats with an electric shock
- 1872, T. Green successfully uses electric shock to start a stopped human heart
- 1878, H. W. von Ziemssen discovers response of heart to regular electrical stimulation
- 1889, J. A. McWilliam experiments with electrical impulses applied to the human heart
- 1899, Defibrillation published in seminal paper by McWilliam
- 1928, Physicist E. H. Booth and surgeon M. C. Lidwell revive a still-born infant
- 1932, A. Hyman invents a hand-cranked device and coins the term “artificial pacemaker”
- 1950, Toronto team employs an AC-powered, external device using vacuum-tube technology
- 1952, P. Zoll keeps a patient alive for 52 hours, following which the patient survives for 6 months
- 1957, E. Bakken and C.W. Lillehei apply a wearable transistorized pacemaker external to the body
- 1958, First use of a fully implantable pacemaker by R. Elmqvist and Å. Senning
- 1959, First use of temporary transvenous pacing for patients awaiting an implanted pacemaker
- 1960, W. Greatbatch and W. C. Chardack employ an improved implantable pacemaker
- 1962, Greatbatch’s U.S. patent 3,051,356 issues, and is licensed to Medtronic, Inc.
- 1970, Medtronic produces an improved pacemaker that becomes a de-facto industry standard
- 1972, First lithium iodide battery powered pacemaker and first hermetically sealed pacemaker
- 1973, Cordis releases the Omni series, the first externally programmable implantable pacemaker
- 1982, A. Rickards introduces rate-modulated pacemakers that adapt the heart rate to demand
- 1988, R. Chirife implants first rate responsive pacemaker using a hemodynamic sensor
- 2005, Biventricular pacing for Cardiac Resynchronization Therapy (CRT) introduced
Bibliography
References of Historical Significance
Thomas Green. 1872. “On Death from Chloroform; Its Prevention by Galvanism”. British Medical Journal, vol. 1 (May 1872): pp. 551–553.
J. A. McWilliam. 1899. “On the Rhythm of the Mammalian Heart”. Journal of Physiology 9, no. 23 (1899): pp. 167-98.
P. M. Zoll. 1952. “Resuscitation of Heart in Ventricular Standstill by External Electrical Stimulation”. New England Journal of Medicine 247 (1952): pp. 768-71.
C. W. Lillehei et al. 1960. “Transistor Pacemaker for Treatment of Complete Atrioventricular Dissociation". Journal of the American Medical Association, April 1960.
W. Greatbatch. 1962. U.S. Patent #3,051,356, issued 28 August 1962
References for Further Reading
O. Aquilina. 2006. "A Brief History of Cardiac Pacing". Images in Paediatric Cardiology 8, no. 2 (Apr-Jun 2006): pp. 17-81
M. S. Eisenberg. 2005. “History of the Science of Cardiopulmonary Resuscitation”. Chapter 1 in J. P. Ornato and M. A. Peberdy, eds., Cardiopulmonary Resuscitation, Humana Press, New York, 2005.
K. Jeffrey. 2001. Machines in Our Hearts: The Cardiac Pacemaker, the Implantable Defibrillator, and American Health Care. Johns Hopkins University Press, Baltimore, 2001.
M. Rowbottom and C. Susskind. 1984. Electricity and Medicine: History of their Interaction. San Francisco Press, San Francisco, 1984
About the Authors
Michael N. Geselowitz is Staff Director of the IEEE History Center. He holds S.B. degrees in electrical engineering and in the anthropology of technology from the Massachusetts Institute of Technology, and M.A. and Ph.D. degrees in the anthropology of technology from Harvard University. His research and publication focus has been on the history and social relations of technology, and he has held teaching and research positions relating to the social study of technology at M.I.T., Harvard, and Yale, including stints as Collections Manager/Curator at Harvard's Peabody Museum and Laboratory Director at MIT’s Center for Materials Research in Archaeology and Ethnology.
Ron S. Leder entered professional biomedical engineering at SUNY Stony Brook in 1977. In 1989 he moved to the University of Wisconsin to develop and direct a sleep research laboratory. Ron has a B.S. in biology, an M.S.E.E. in digital systems, and a Ph.D. in E.C.E. He worked as assistant editor on the Wiley Encyclopedia of Electrical and Electronics Engineering. Ron has served as chair of the EMB History Committee. He is currently a professor of electrical engineering (biomedical) at Universidad Nacional Autonoma de Mexico and is local EMB chapter chair. He has lived in Mexico City since 1999.